To our great distress, it is currently IMPOSSIBLE to accurately count the deaths caused by medical error — that was before the COVID-19 vax injured and killed us.
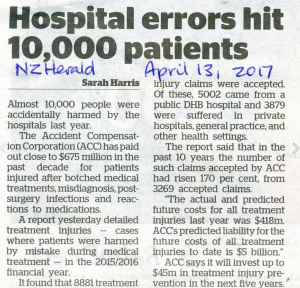
18,000 patients killed? 18,000 patients killed in one year? Yes, killed. Yes, in one year. But that was just 1995. It’s increasing each year. You better believe it, you are not safe in our hospitals. Again, this was before our governments forced us or else to be vaccinated against COVID-19; a vaccine that was not tested for efficacy.
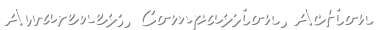
Australia’s Minister for Health, the Hon Dr Carmen Lawrence MP, announced this abominable figure of 18,000 deaths in one year in Parliament on 14 June 1995. Then it was peer reviewed and published in The Medical Journal of Australia in November 1995. The figure is actually extrapolated from a statistically valid sample of 14,179 hospital admissions.
We believe it underestimates the horrifying magnitude of medical error. Over a quarter of a century later, we are still waiting for a standardised, accurate, centralised, compulsory system for recording the death toll. When this exists, it will expose hospital managements to public scrutiny. Even more important, it will give the medical system the opportunity to learn from its mistakes – and prevent them.
If you think we are being alarmist, consider this: Medical error is totally ignored as a cause of death by the Australian Bureau of Statistics (ABS). It should be at least second from the top.
 click to enlarge
click to enlarge For a comprehensive overview read:
An analysis of the causes of adverse events from the Quality in Australian Health Care Study
A more recent Victorian study gives more cause for alarm
At this rate, the national tally of medical adverse events would be over 54,000 leading to 13,500 preventable deaths.
18,000 dead? 13,500 dead? Nobody knows for sure. But every study shows that the suffering and death caused by hospital treatment far exceed the road toll* — a national, shameful scandal.
See MJA: The incidence and cost of adverse events in Victorian hospitals 2003–2004
* ABS: Transport accidents: 1,402 deaths registered in 2008.
“Case-mix” turned out to be case-shambles
Around two-thirds of senior clinicians were of the view that government reforms have contributed to a deterioration in the quality of clinical care in their respective hospitals.
The main reasons for the decline were increased economic pressures caused by the drive for shorter lengths of stay in hospitals and increased patient throughput, a higher proportion of beds occupied by seriously ill patients and staff reductions.
Increased patient acuity, reduced patient/staff ratios, a reduction of experienced staff and not enough time for more supervision have contributed to the increased proportion of adverse events.
Increased workloads lead to less attention to detail resulting in greater opportunity for adverse incidents. Less time and more haste in planning and implementing procedures and treatments are also contributing factors to adverse events.
…Acute Health Services Under Casemix — A Case of Mixed Priorities. Tabled in Parliament of Victoria, Australia, May 1998.